Total Hip Replacement
Home > Condition & Treatment Map > Hip & Pelvis Conditions & Treatments > Total Hip Replacement
Total Hip Replacement: An Introduction
Total hip replacement, also known as hip arthroplasty, is a surgical procedure to replace a worn-out or damaged hip joint with an artificial joint (prosthesis). This surgery is usually performed to relieve pain and improve function in patients with severe hip arthritis or hip joint damage.
At Victorian Bone and Joint Specialists (VBJS), our highly skilled and experienced surgeons are dedicated to providing exceptional care for patients requiring total hip replacement. Located in Melbourne, our fellowship-trained orthopaedic surgeons utilise the latest techniques and technologies to ensure the best possible outcomes for our patients. With a commitment to personalised care and advanced surgical expertise, VBJS is a leading centre for hip replacement surgery in Melbourne. Our modern facilities and post-operative care services support patients from initial consultation through to recovery, ensuring a smooth and successful surgical experience.
Total hip replacement, also known as total hip arthroplasty, is a common procedure where a faulty joint is replaced with an artificial counterpart (a hip prosthesis). Hundreds of thousands of hip replacements are completed around the world every year. With proper care and activity modification, the prosthetic joint can last 15-20 years or more. Read More
When completed successfully, a total hip arthroplasty surgery will reduce the pain and improve the functionality of a damaged or arthritic hip joint.
How Total Hip Replacement Surgery Works
The hip joint comprises the ball (femoral head) and socket (acetabulum). In a full hip replacement, an experienced surgeon will replace the damaged femoral head with a metal or ceramic ball. This ball is attached to a metal stem, which is carefully inserted into the femur. The socket is replaced with a metal cup, often lined with plastic or ceramic, which facilitates smooth movement.
There are, however, several types of hip replacement. For example, a partial hip replacement involves a replacement of the ball of the hip joint but leaves the socket intact. Another way that hip replacement surgery can vary is the surgical approach. For example, during an anterior approach, a surgeon can make an incision from the front of the hip, allowing them to work between the muscles. A posterior approach will require careful cutting through the gluteus maximus muscle at the back of the hip. The procedure shouldn't be painful, as the surgeon will use anaesthetic.
Which surgery and approach will be recommended for you will depend on the state of your hip. There are many different factors that contribute to hip damage. For example, osteoarthritis is the most common cause resulting from wear and tear. Rheumatoid arthritis (another arthritis variant), an autoimmune disease, can also lead to joint inflammation and damage. Post-traumatic arthritis may develop following hip injuries, while avascular necrosis occurs due to insufficient blood supply to the bone tissue.
Severe hip fractures that cannot be repaired with other methods may necessitate hip arthroplasty. Additionally, childhood hip conditions like hip dysplasia can progress into joint damage over time. During an initial consultation, a specialist will examine your hip joint and suggest a treatment plan.
One question we're frequently asked is how long it will take to recover from hip replacement surgery. The answer is multifaceted, as wounds typically heal within two weeks. You should notice significant improvements in your hip replacement within the first 6 weeks. However, full recovery can take up to 3 months, with continued improvements up to a year.
The time it takes to return to work and sports after a total hip replacement procedure varies. Office work can usually resume within 4 weeks, while manual labour may take up to 12 weeks. Low-impact, joint-friendly activities like swimming and cycling can typically start 6-12 weeks post-surgery, while you should avoid high-impact sports for at least 12 weeks. The specific recovery timeline depends on individual factors, including pre-surgery function, type of hip replacement and post-operative progress.
One way that the healing process can be accelerated is if the surgeon uses total hip replacement technology. The total hip replacement technology landscape is constantly innovating. For example, robotic hip replacement is an advanced technique that uses a robotic arm to assist in precise hip implant placement. If you feel robotic hip replacement could be a good option for you, speak to your specialist.
What are the Advantages and Disadvantages of Hip Resurfacing?
Examining Hip Resurfacing in Detail
During a traditional hip replacement, the surgeon will replace the damaged joint with a metal ball and a plastic socket through a large incision in the skin. In comparison, hip resurfacing uses metal implants to replace the outer surfaces of the hip joint, including the ball and socket, while leaving the underlying bone intact.
More particularly, instead of removing the entire femoral head, a portion is trimmed and then capped with a smooth metal covering. The covering - often made from materials like titanium - allows for a more natural interaction between the femur and the acetabulum (the two main components of the hip joint). However, like traditional hip replacement (also known as an arthroplasty), the damaged bone and cartilage within the acetabulum (the hip socket) are removed and replaced with a metal shell.
If you're exploring hip resurfacing as a way to treat hip pain or loss of mobility, you might take a measured approach: balancing the advantages and disadvantages to make a fully informed decision.
It's especially important to consider the advantages and disadvantages of hip resurfacing compared to traditional hip replacement. Hip resurfacing versus hip replacement is a controversial topic among some surgeons, so it's important to consider the advantages and disadvantages from your perspective.
The advantages of hip resurfacing include the decreased risk of dislocation. Hip resurfacing uses a larger ball, emulating the size of the standard hip ball. Consequently, some surgeons believe that hip resurfacing leads to a lesser chance of relocation. However, dislocation is also subject to external factors, such as how the surgery is performed and the type of implant.
Another reason that hip resurfacing is believed to decrease the risk of dislocation is because it allows for more natural walking. Some research substantiates the idea that hip resurfacing contributes towards a more natural pattern of walking. These differences are very minor, however, and should not constitute the sole basis of your decision.
Both hip resurfacing and replacement can last up to 15-20 years before requiring replacement. Some surgeons believe that exchanging the hip implants is more straightforward after resurfacing - compared to exchanging the implants after hip replacement.
The ease of replacement and the decreased risk of dislocation must be balanced against the suggested disadvantages of hip resurfacing. These include the risk of adverse local tissue reaction, which results from the metal surfaces rubbing together and releasing ions (which are small particles of metal). These ions inflame the tissue around the joint, inducing discomfort, pain and swelling. Though it is treatable via revision surgery, these ions can enter the bloodstream and be circulated around the whole body. For that reason, some surgeons eschew hip resurfacing.
Another concern associated with hip resurfacing is the risk of femoral neck fracture. In the vast minority of hip resurfacing cases, the femoral neck may fracture after the operation. The solution to femoral neck fracture is to have a traditional hip replacement, which may motivate some patients to elect for a hip replacement initially.
Although a traditional hip replacement procedure involves removing the femoral neck, fractures may still occur around the site of the hip replacement, meaning it is not an infallible solution.
Who is a Good Candidate for Hip Resurfacing Treatment?
Firstly, you'll know that it's time to seek a surgeon's opinion when you start to experience the following symptoms:
- Swelling.
- Hip pain.
- A decreased range of motion (or how far you can move your hip without discomfort).
- Stiffness
- Limited mobility (i.e. difficulty walking or moving).
- Instability (or the sensation of feeling unsteady or unbalanced on your hip).
Your surgeon will carefully examine your hip joint, taking scans where necessary and asking about your symptoms. Then, depending on your suitability for hip replacement or resurfacing, they'll recommend a treatment.
In a nutshell, younger patients (i.e. typically under 60 years old), with larger frames, often male, and strong, healthy bones may be ideal candidates for hip resurfacing. The size of the bones is also a significant factor - as men naturally often have larger bones, they are more likely to be considered suitable candidates for hip resurfacing.
Other candidates, such as those with brittle and/or aged bones, are more likely to experience complications like femoral head fracture. A reputable surgeon will quickly determine your suitability for hip resurfacing.
How Should I Prepare for Hip Resurfacing Treatment?
Your surgeon will inform you if and when you should stop eating and drinking the day before your surgery. They may also advise on the medications that you can and cannot take. Note that before the hip resurfacing treatment, they might administer certain tests to affirm that you're ready for surgery - such as physical exams and blood tests.
It is the hip resurfacing surgeon's job to ensure that you're physically ready and fully informed ahead of your hip resurfacing. For more information, get in touch with our friendly team.
How does Hip Resurfacing Work?
The hip resurfacing process follows a number of steps that 'resurface' your femur and realign your hip joint in one clinical procedure. Let's break it down:
- Make the most minimal possible incision near your hip.
- Remove damaged cartilage and bone from the hip socket by levering the damaged or worn cartilage on the surface of the acetabulum.
- Place a prosthetic acetabulum in the socket. The implant is a cup-shaped component designed to adhere to the dimensions of your natural acetabulum closely.
- Reshape the top of your femur to fit the new socket. This is the 'resurfacing' part of the operation.
- Place a metal or ceramic cap on the femur. The surface of the cap will be smooth and durable.
- Realign the hip joint and connect the resurfaced femur to the prosthetic socket. More specifically, the surgeon will meticulously adjust the position of the femoral head in relation to the prosthetic acetabulum. The result is a properly aligned and stabilised hip joint. By stabilising the hip joint, the surgeon helps to prevent future dislocation, reduce swelling and aid with natural walking.
End to end, the process will take somewhere between one and two hours. During the operation, you should not feel pain, as the surgeon will apply local anaesthetic. As an outpatient procedure, after the surgeon has conducted a medical exam and drawn up a physical therapy assessment, you will be free to go home and rest.
Managing the Pain After Hip Resurfacing
Your surgeon will work with you to ensure that your pain is managed through suitable medications. These medications may include prescription pain medication, acetaminophen (also known as Tylenol and Panadol) and anti-inflammatories. If you're experiencing severe pain despite taking your assigned medications, your surgeon will adjust the dose to ensure minimal discomfort.
How Will I Recover From Hip Resurfacing Treatment?
Full recovery from hip resurfacing typically takes several months. Your surgeon may encourage you to start moving and bearing weight on your hip soon after surgery, possibly even the next day. Assistive devices like crutches or a walker may be necessary for a few weeks, but recovery is expected after approximately six weeks. If your hip pain is manageable enough to allow you to continue with your work or studies, you may only require a short recovery period of one to two weeks.
For guidance on safe movement after surgery, consult with your surgeon or physical therapist. They can provide specific advice on everyday activities like walking, sitting, standing, using the bathroom, bathing, dressing, and navigating stairs.
Physical therapy is often recommended for several weeks following hip resurfacing. A physical therapist can provide exercises to strengthen your hip muscles and improve your range of motion during the recovery process.
Hip Resurfacing vs. THR - From a Hip Resurfacing Surgeon's Perspective
We've already discussed the advantages and disadvantages of hip resurfacing, but let's directly compare them to Total Hip Replacement (THR).
After healing, hip resurfacing patients generally find they can experience a greater range of physical activities (such as running, jumping, etc.) in comparison to THR patients who are generally advised to stick to lower-impact activities, such as swimming and walking. Hence, hip resurfacing may seem like a more attractive option to younger patients who are keen more for a more satisfying recovery. Some surgeons consider hip resurfacing a safer and more durable long-term option.
As aforementioned, femoral neck fractures and metal ionisation are risks that may deter some patients. If in doubt about the risks, do not hesitate to seek a professional opinion from your surgeon.
There are also the standard risks associated with both hip replacement and hip resurfacing operations, such as infection, blood clots and risks to nerve damage. However, these only occur in a tiny percentage of patients undergoing surgery.
Victorian Bone and Joint Specialists (VBJS) is proud to be highly qualified hip resurfacing specialists in Melbourne. Our hip surgeries have alleviated the discomfort of hundreds of people around the Melbourne area. Plus, we offer flexible referral options that mean you can see us quickly on your own terms.
Get in Touch to Find out More About Hip Arthroplasty
Victorian Bone and Joint Specialists (VBJS) boasts a team of skilled and experienced surgeons who are dedicated to providing exceptional care during hip replacement procedures.
Located in Melbourne, our fellowship-trained orthopaedic surgeons leverage the latest techniques and technologies. The result? The best possible outcomes for our patients, every time.
We'll guide you through the hip replacement process, from the initial consultation to successful recovery. Our friendly and personable surgeons will ensure you have all the necessary information to make informed decisions along the way.
Get in touch to discover how we can support you in your hip replacement journey. Read Less
Anatomy
The hip joint consists of the ball (femoral head) and socket (acetabulum). In a hip replacement, the damaged femoral head is replaced with a metal or ceramic ball attached to a metal stem, which is inserted into the femur. The socket is replaced with a metal cup, often lined with plastic or ceramic, to allow smooth movement.
Reasons for Total Hip Replacement
Osteoarthritis: The most common reason, causing wear and tear of the joint.
Rheumatoid Arthritis: An autoimmune disease causing joint inflammation and damage.
Post-Traumatic Arthritis: Arthritis following an injury to the hip joint.
Avascular Necrosis: Loss of bone tissue due to a lack of blood supply.
Hip Fractures: Severe fractures that cannot be repaired with other methods.
Childhood Hip Diseases: Conditions like hip dysplasia leading to joint damage over time.
Different Approaches
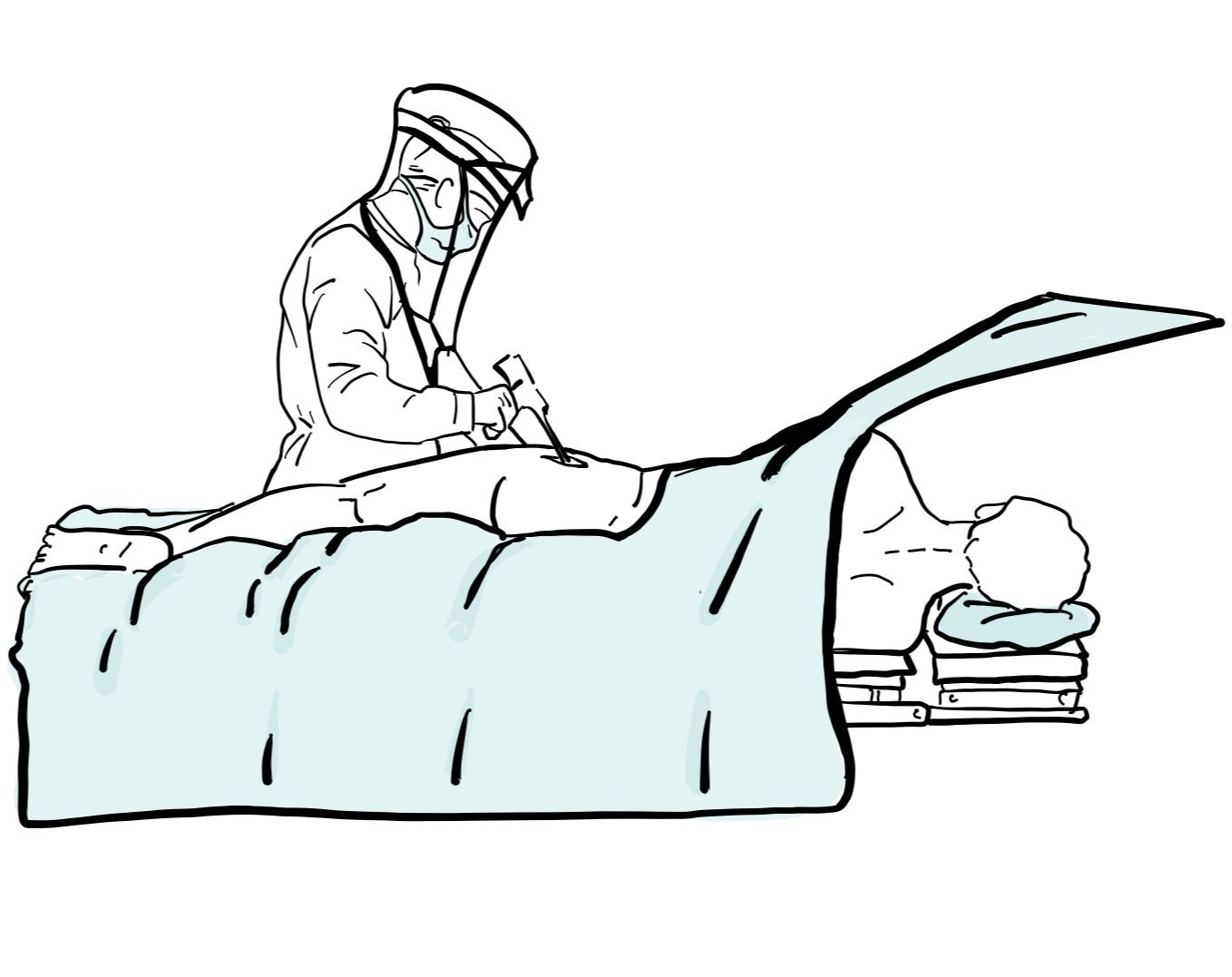
Anterior approach: An incision is made at the front of the hip, allowing the surgeon to work between muscles without detaching them.
Posterior approach: An incision is made at the back of the hip, which requires cutting through the gluteus maximus muscle.
Each approach has specific precautions and recovery guidelines, and the choice often depends on the surgeon's experience, the patient's anatomy, and overall health.
Robotic Hip Replacement
Robotic hip replacement is an advanced technique using a robotic arm to assist in precise hip implant placement. The system creates a 3D model of the patient's hip from pre-operative imaging, allowing for accurate surgical planning. The surgeon controls the robotic arm to ensure precision and consistency. This method aims to improve implant alignment and fit, potentially leading to better outcomes. Discuss with your surgeon if robotic hip replacement is suitable for you.
Preparing for Surgery
Medical Evaluation: A thorough evaluation by your surgeon and primary care doctor to assess your overall health and readiness for surgery.
Medications: Inform your doctor about all medications you are taking. Some may need to be stopped before surgery.
Pre-Surgical Tests: Blood tests, X-rays, and other imaging studies.
Home Preparation: Arrange for help at home during your recovery period. Make necessary modifications to make your home safer and more accessible.
Fasting: You may need to fast (not eat or drink) for several hours before the surgery.
The Surgery
Anaesthesia: You will be given general anaesthesia (you will be asleep) or spinal anaesthesia and sedation (you will be sedated but numb from the waist down). This will be discussed with you by our anaesthetist.
Procedure: The surgeon makes an incision over the hip joint, removes the damaged bone and cartilage, and replaces it with the prosthetic joint.
Duration: The surgery usually takes 1-2 hours.
After Surgery
Recovery Room: You will return to the recovery room where your vital signs will be monitored.
Pain Management: Medications will be provided to control pain.
Physical Therapy: You will start physical therapy soon after surgery to help regain movement and strength.
Hospital Stay: Most patients stay in the hospital for 2-3 days.
Recovery and Rehabilitation
Physical Activity: Gradual increase in activity is crucial. Follow your physical therapist's instructions.
Assistive Devices: You may need crutches, a walker, or a cane for a few weeks.
Avoid Certain Movements: Avoid crossing your legs, bending your hip more than 90 degrees, and twisting your leg inward.
Exercise: Regular exercises to strengthen your hip and improve flexibility.
Driving: You can typically resume driving 6 weeks after surgery, depending on your recovery and your doctor's advice.
Post-Operative Care
Pain Relief:
It is normal to have some pain or discomfort after surgery. You will be given pain relief medications such as NSAIDs and opiates.
Avoid driving, drinking alcohol, or performing duties requiring concentration while on opiate pain medications.
Icing:
Some patients find that icing their hip replacement after surgery can improve pain relief and reduce swelling
Use ice packs consistently for the first 24-48 hours to reduce swelling.
After this period, apply ice packs 3-4 times per day for 30 minutes until swelling subsides.
Bowel and Bladder Function:
Pain medications can reduce bowel function, so it is important to take stool softeners like Coloxyl and Senna or Movicol daily while you are taking opiates.
Maintain a high-fiber, high-protein diet to assist with bowel function.
Blood Tests and X-Rays:
X-rays will be taken the day after surgery to check the alignment of your hip.
Blood tests may be conducted as needed based on your physician and surgeon's assessment.
Discharge Home:
Most patients stay in the hospital for 2-3 days after surgery.
You will be discharged with pain relief medications and a rehabilitation plan.
Weight Bearing:
Most patients can full weight bear as tolerated on their hip replacement immediately after surgery. Your surgeon will advise you on your specific weight bearing status.
Blood Clot Prevention:
Medication such as Clexane or Aspirin may be prescribed.
Wear compression stockings for 14 days.
Early mobilization and staying hydrated are essential to prevent blood clots.
Risks and Complications
Infection: Antibiotics are given to prevent infection.
Blood Clots: Blood-thinning medications may be prescribed.
Dislocation: The new joint can dislocate if not careful with certain movements.
Leg Length Inequality: Small differences in leg length can occur.
Nerve and Blood Vessel Injury: Rare but possible.
Wear and Tear: The prosthetic joint may wear out over time, requiring revision surgery.
Long-Term Outcomes
Most patients experience significant pain relief and improved mobility.
The prosthetic joint can last 15-20 years or more with proper care and activity modification.
Regular check-ups with your doctor to monitor the condition of the prosthetic joint.
Frequently Asked Questions (FAQs)
Q: Which implants do surgeons use?
A: Surgeons use a variety of implants depending on the shape of your bones and the type of arthritis you have. Implants with excellent results on the Australian Joint Replacement Registry are used.
Q: Am I too young for hip replacement surgery?
A: Hip arthritis affects people of many ages, and hip replacement surgery is effective for pain relief in both young and older patients. If hip preservation options have failed, then total hip replacement may be a viable option.
Q: When can I walk after a posterior total hip replacement?
A: Full weight-bearing and walking are usually allowed immediately after surgery, typically aided by crutches. Patients usually begin mobilizing on the first day after the operation. Your surgeon will advise what your weight bearing status is.
Q: When can I work after a posterior total hip replacement?
A: Return to work varies depending on the type of work. Most people can return to office work within 4 weeks, while more strenuous manual work may require up to 12 weeks.
Q: When can I play sports after a total hip replacement?
A: Your ability to return to sports will depend on your pre-surgery function, your specific hip replacement, and your progress post operatively. Typically. low-impact activities like cycling and swimming can be started 6-12 weeks after surgery. High-impact activities should be avoided for at least 12 weeks.
Q: How long will it take to heal after a posterior total hip replacement?
A: Wounds typically heal in 14 days, and your hip replacement will have significant improvement within the first 6 weeks. Full recovery can take up to 3 months, with continued improvements up to a year.
Q: How much pain will I experience after a total hip replacement?
A: Most patients experience minimal pain after surgery due to local anaesthetics used during the procedure.
Q: Will I set off metal detectors at airports?
A: It is possible, depending on the sensitivity of the detectors. Inform security personnel if you have had a hip replacement.
Note: This information sheet is for educational purposes and is not a substitute for professional medical advice. Always follow your healthcare provider's instructions and guidance.