Periacetabular Osteotomy (PAO) Handbook and Pathway
Home > Condition & Treatment Map > Hip & Pelvis Conditions & Treatments > Periacetabular Osteotomy (PAO) Handbook and Pathway
Overview
What is a PAO?
A PAO is a procedure which is done to correct deformity of the pelvis, typically due to hip dysplasia or other structural problems. Most patients who undergo PAO surgery are less than 35yrs of age and they have hip pain. PAO surgery has been shown to be highly effective at treating hip pain and delaying arthritis in symptomatic patients.
PAO Surgery
Many patients with hip dysplasia (shallow socket) have other problems within the joint (cartilage tears) and/or may have a deformity of the femoral head (ball) of femur bone. Commonly, these other problems are treated during or after the PAO procedure.
Occasionally there is also a deformity of the femur that must be corrected at the time of surgery by a proximal femoral osteotomy (PFO). This involves cutting and repositioning the upper portion of the femur (thigh) bone. If this is needed, a second incision is made on the outside of the hip and the femur is repositioned and fixed with a rod, or a metal plate and screws.
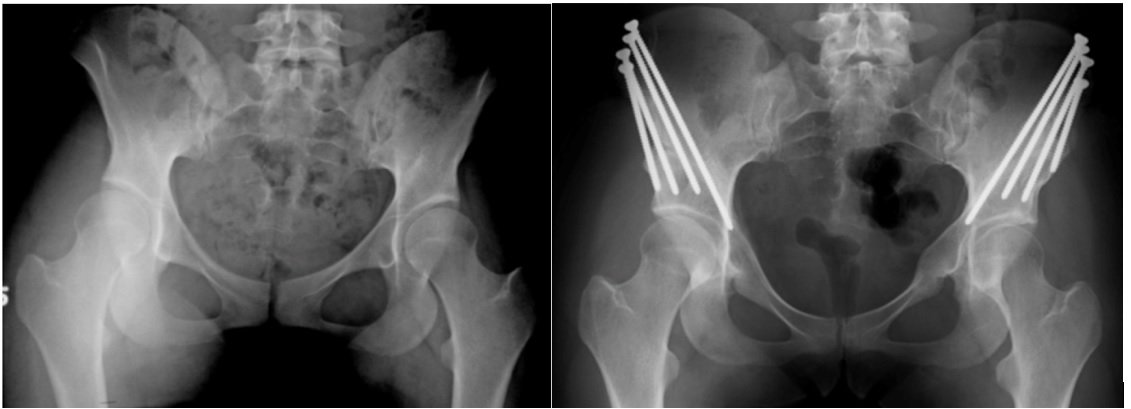
X-rays of a young female with bilateral hip dysplasia are shown (left). She had PAOs done to both hips and has an excellent result in both hips.
What to Expect
After PAO, there is a variable amount of pain and swelling, which can vary between individuals. This usually diminishes after several weeks. It is helpful to keep the leg elevated and to apply ice regularly.
Numbness: Most patients develop numbness down the outside of the leg/thigh – this relates to nerve stretching, and it typically goes away after several months.
What to Report Immediately
If you experience any of the following, contact VBJS immediately, or his mobile on 0475582244:
Persistent fever
Wound redness, drainage, or increased skin temperature around the incision
Increasing numbness
Sudden increase in pain or swelling
Deep calf pain and/or swelling
Shortness of breath
Post Operative Care
You should have a post-op appointment scheduled in 14 days. If you do not, contact VBJS.
Pain Relief
If you had a nerve block, your leg may be numb for 12-18 hours. Although you may not be having much pain, start taking your pain medication 6 hours after surgery.
You will have a painbuster catheter inserted into the wound – this provides a trickle of local anaesthetic for 48hrs
You will routinely be prescribed Palexia and Endone (2 weeks) which is a narcotic pain medication for your post-op pain control. This is addictive and you should aim to cease it as soon as possible.
Take the Palexia regularly for the first one-two weeks. Then take the Endone for breakthrough pain as required every 4 hours. It is better to be pain free and be able to do the exercises rather than be in pain and not be able to do any exercise.
Use the medicine as prescribed and do not drive, drink alcohol, or perform duties that require concentration (i.e. school or work) while on the narcotic medication.
Wound Care
You may remove the dressing in 12 days and apply band aids to cover stitches. Please use steri strips when dressings are removed (white tapes across wound). It is OK if they fall off.
You may shower in 3 days with the incision covered. Keep it clean and dry.
Do not get into a tub or pool until the wound is reviewed at 2 weeks post op.
You have dissolvable sutures, No suture removal is necessary
Icing
It is recommended that you ice your hip. Ice in a bag with cloth covering can be used fairly consistently for the first 24 to 48 hours to help diminish the swelling. After the 48 hour period, if it is comfortable for you, you may apply ice packs to the hip 3-4 times per day for 30 minutes until swelling is resolved.
Bowels and Bladder Function
All patients have a catheter when they wake up from surgery. This is typically removed at day 2 post op.
It is important that regular medications are given to soften bowel contents and typically coloxyl and senna is given or Movicol daily for the first two weeks, as the pain medications can reduce bowel function post operatively.
CPM – Knee Bending Device
Post operatively you will be placed into a CPM machine to help bend and straighten the knee for 4-6hrs per day from 30-70°. This is to maintain your range of movement and prevent scarring.
Crutches
You may partially weight bear (20%) of your body weight for 4 weeks.
After 4 weeks if you feel comfortable you can transition to one crutch and then after review at 6 weeks wean off the one crutch.
Weight bearing with crutches in a heel à toe gait until 6-8 weeks when you can wean off the crutches is important. Hydrotherapy may be useful from 4 weeks.
Blood Tests and X Rays
You will undergo blood tests day 1 and x-rays day 2-3 to check the alignment of your hip.
Blood Clot Prevention
Blood clots are rare after PAO surgery, but they can be serious. You will undergo the following preventative strategies:
Medication – Xarelto is typically given for 14days
Compression stockings – typically for 14days
Early mobilisation – the quicker patients get up and move, the faster blood gets moving and the lower the risk of blood clots
Remaining hydrated – if you remain well hydrated this can reduce your risk of blood clots
Other Medication and Treatments
A prescription may be provided for Valium if you are having spasms and Indocid (an anti-inflammatory). Use as prescribed unless contradicted. Do not drive, operate machinery, or drink alcohol while on valium. Valium is used for muscle spasms and Indocid or anti-inflammatories are used for prevention of heterotopic ossification (excess bone re-formation).
Driving
You may not drive at least until your post-op visit when you and Dr Slattery can make a decision, this is based upon your pain, medications, leg strength and also which leg has been operated on.
Post Operative Review
You will be reviewed at 2 weeks post op by Mr Slattery – please call VBJS to make an appointment if you do not have one scheduled.
Physiotherapy
You will be seen on the wards twice daily by the physiotherapy team. They will help you with:
Getting in and out of bed
Using crutches
Helping you with walking and gait retraining
Setting up and Using CPM
You can arrange to be seen by PT within the first week of discharge from surgery. You will continue therapy, with specific therapist instructions, at the first post-operative visit. You may wish to set up an appointment with physiotherapy in advance (2-3 sessions/week).
For the first two weeks until formal physical therapy, you may do the following exercises:
Limit External rotation of the hip to 10°, No restrictions on internal rotation. Hip flexion to 90°
Ankle pumps: Move ankle up and down. 30 reps, 3 times daily.
Hip Pendulum: Stand on step supported by non operative leg, allow operative leg to hang off edge, gently move leg in circular motion clockwise and counter clockwise x 10, 3 times daily.
Other Physiotherapy Information
No weight lifting or water therapy during first two weeks.
If an exercise is very painful, stop doing it or do it within the limits of motion that is not painful.
Major therapy gains are not made in the first two weeks – this is mainly a recuperative period.
Exercise Bike as a CPM
A stationary exercise bike should be hired or sourced if possible
Start the bike for 10 mins a day for the first week bending the hip 30-70°, advance to 0-70° as tolerated. By week 4 you should aim to complete 20 mins per day
Set the machine at low to medium speed with no resistance for the 3rd week
You should use the machine for the first 21 to 28 days
Physiotherapy Protocol Post-PAO
PHASE I — IMMEDIATE REHABILITATION – Usually 2-4 weeks
Goals
Protect integrity of repaired tissue
Restore ROM within restrictions
Diminish pain and inflammation
Prevent muscular inhibition
Precautions
Do not push through hip flexor pain
Specific ROM restrictions (surgery dependent)
Weight-bearing restrictions – Partial Weight Bearing with Crutches for 4-6weeks (20%)
Criteria for Progression to Phase II
Minimal pain with all phase I exercise
ROM>75% of the uninvolved side
Proper muscle firing patterns for initial exercises
Do not progress to phase II until full weight bearing is allowed
Specific Exercises:
Ride bike comfortable for 20 mins/day
Straight leg raises (Rectus)
Clams or Side leg raises (Abductor strengthening)
Supine abduction in bed
Prone lying for psoas stretching
PHASE II — INTERMEDIATE REHABILITATION –4-8 weeks
Goals
Protect integrity of repaired tissue
Restore full ROM
Restore normal gait pattern
Progressively increase muscle strength
Precautions
No ballistic or forced stretching
No treadmill use
Avoid hip flexor/joint inflammation
Criteria for Progression to Phase III
Full range of motion
Pain-free/normal gait pattern with aids
Hip flexion strength >60% of the uninvolved side
Hip add, abd, ext, IR, ER strength >70% of the uninvolved side
Specific Exercises
Ride bike for 40mins/day with resistance
Hydrotherapy
Weight Bear as tolerated with two then one crutch
Double one third knee bends
Side bridges
Side Leg Raises
Straight Leg Raises
Advanced bridges
PHASE III — ADVANCED 8 weeks to 3 months
Goals
Restoration of muscular endurance/strength
Restoration of cardiovascular endurance
Optimize neuromuscular control/balance/proprioception
Precautions
Avoid hip flexor/joint inflammation
No ballistic or forced stretching/strengthening
No treadmill use
No contact activities
Criteria for Progression to Phase IV
Hip flexion strength >70% of the uninvolved side
Hip add, abd, ext, IR, ER strength >80% of the uninvolved side
Cardiovascular fitness equal to preinjury level
Demonstration of initial agility drills with proper body mechanics
Specific Exercises
Treadmill – inline running for 10 mins per day. Increase incline
Side steps
Side pivots
Single leg knee bends
Plyometrics
Advanced strength training
Side to side lateral agilities
PHASE IV— SPORT-SPECIFIC TRAINING
Criteria for Full Return to Competition
Full pain-free ROM
Hip strength >85% of the uninvolved side
Ability to perform sport-specific drills at full speed without pain
Completion of functional sports test